 Introduction As medical care evolves, clinicians and researchers are exploring the use of technology to improve the quality and effectiveness of medical care. In this regard, technology is being used to deliver precision medicine. This form of medicine is a new approach that focuses on using genomic, environmental and personal data to customize and deliver precise form of medical treatment. Hence the name ‘precision medicine’. One of the most influential factors, in recent years, in delivering precision medicine has been Artificial Intelligence (AI). In specific one of its forms Machine Learning (ML). ML, which uses computation to analyze and interpret various forms of medical data to identify patterns and predict outcomes has shown increasing success in various areas of healthcare delivery. In this article, I discuss how computer vision and natural language processing, which use ML can be used to deliver precision medicine. I also discuss the technical and ethical challenges associated with the approaches and what the future holds if the challenges are addressed. Image Analysis Various forms of medical imaging techniques like X-rays, CT, MRI and Nuclear imaging techniques are being used by clinicians to assist their diagnosis and treatment of various conditions ranging from cancers to simple fractures. The importance of these techniques in devising specific treatments has become critical in recent years. However, the dependency on a limited subset of trained medical specialists (Radiologists) to interpret and confirm the images has meant in many instances increase with the diagnosis and treatment times. The task of classifying and segmenting medical images can not only be tedious but take a lot of time. Computer Vision (CV), a form of AI that enables computers to interpret images and relate what the images are, has in the recent years shown a lot of promise and success. CV is now being applied in medicine to interpret radiological, fundoscopic and histopathological images. The most publicized success of recent years has been the interpretation of retinopathy images to diagnose diabetic and hypertensive retinopathy. The use of CV, powered by neural networks (an advanced form of ML), is said to take over the tedious task of segmenting and classifying medical images and enable preliminary or differential diagnosis. This approach is stated not only to accelerate the process of diagnosis and treatment but also provide more time for the radiologists to focus on complex imaging interpretations. Natural Language Processing As with CV, Natural Language Processing (NLP) has had a great impact on society in the form of voice assistants, spam filters, and chat-bots. NLP applications are also being used in healthcare in the form of virtual health assistants and in recent years have been identified to have potential in analyzing clinical notes and spoken instructions from clinicians. This ability of NLP can lessen the burden for busy clinicians who are encumbered by a need to document all their patient care in electronic health records (EHRs). By freeing up the time in writing copious notes, NLP applications can enable clinicians to focus more of their time with patients. In the recent period NLP techniques have been used to analyze even unstructured (free form and written notes) data, which makes it useful in instances where written data is not available in the digital form or there are non-textual data. By integrating NLP applications in EHRs, the workflow and delivery of healthcare can be accelerated. Combination of Approaches Precision medicine is premised on customization of medical care based on individual profile of patients. By combining NLP and CV techniques, the ability to deliver precision medicine s greatly increased. For example, NLP techniques can scroll through past medical notes to identify previously diagnosed conditions and medical treatment and present the information in a summary to doctors even as the patient presents to the clinic or to the emergency department. Once in the clinic or emergency department, NLP voice recognition applications can analyze conversation between the patient and clinicians and document it in the form of patient notes for the doctor to review and confirm. This process can free up time for the doctor and ensure accuracy of notes. As the doctor identifies the condition affecting the patient and relies on confirmation through relevant medical imaging, automated or semi-automated CV techniques can accelerate the confirmation process. Thus, a cohesive process that can accelerate the time in which the patient receives necessary medical treatment. Let us see how this works in a fictitious example. Mr Carlyle, an avid cyclist, meets with an accident on his way to work when an automobile swerves into the bike lane and flings him from his bicycle. The automobile driver calls in an ambulance when he notices Mr Carlyle seated and grimacing with pain. The ambulance after arrival having entered his unique patient identifier number, which is accessed from his smartwatch, rushes him to the nearest emergency department. The AI agent embedded in the hospital’s patient information system identifies Mr Carlyle through his patient identifier number and pulls out his medical details including his drug allergies. This information is available for the clinicians in the emergency department to review even as Mr Carlyle arrives. After being placed in an emergency department bay, the treating doctor uses an NLP application to record, analyze and document the conversation between her and Mr Carlyle. This option allows the doctor to focus most of her time on Mr Carlyle. The doctor suspects a fracture of the clavicle and has Mr Carlyle undergo an X-ray. The CV application embedded in the imaging information system has detected a mid-shaft clavicular fracture and relays the diagnosis back to the doctor. The doctor, prompted by an AI clinical decision support application embedded in the patient information system, recommends immobilization and a sling treatment for Mr Carlyle along with pain killers. His pain killer excludes NSAIDs as the AI agent has identified he is allergic to aspirin. Challenges The above scenario while presenting a clear example of how AI, in specific CV and NLP applications, can be harnessed to deliver prompt and personalized medical care is yet contingent on the technologies to deliver such outcomes. Currently, CV techniques have not achieved the confidence of regulatory authorities nor clinicians to allow automated medical imaging diagnosis (except in minor instances such as diabetic retinopathy interpretation) and neither are NLP applications embedded in EHRs to allow automatic recording, analysis and recording of patient conversations. While some applications have been released in the market to analyze unstructured data, external validation and wide acceptance of these type of applications are some years away. Coupled with this technical and regulatory challenges is the ethical challenges of enabling autonomy of non-human agents to guide and deliver clinical care. Further issues may arise due to the use of patient identifiers to extract historical details even if it is for medical treatment if the patient hasn’t consented so. Yet, the challenges can be overcome as AI technology improves and governance structures to protect patient privacy, confidentiality and safety are established. As focus on the ethics of application of AI in healthcare increases and technological limitations of AI application get resolved, the fictitious scenario may become a reality not too far into the future. Conclusion There is a natural alignment between AI and precision medicine as the power of AI methods such as NLP and CV can be leveraged to analyze bio-metric data and deliver personalize medical treatment for patients. With appropriate safeguards, the use of AI in delivering precision medicine can only benefit both the patient and clinician community. One can based on the rapidly evolving AI technology predict the coming years will see wider adaption of precision care models in medicine and thus AI techniques.
1 Comment
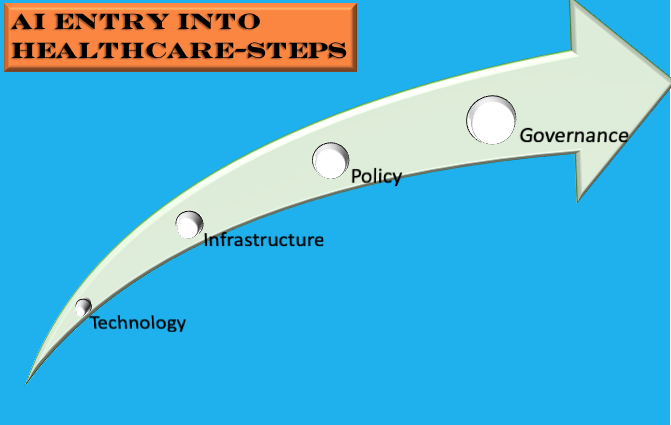
With recent developments in regard to AI in Healthcare, one could be mistaken that the entry of AI in healthcare is inevitable. Recent developments include two major studies, one where machine learning classifiers used for hypothetico-deductive reasoning were found to be as accurate as paediatricians and the other one where a deep-learning based automated algorithm outperformed thoracic radiologists in accuracy and was externally validated in multiple sites. The first study is significant in that machine learning classifiers are now proven to be not only useful for medical imaging interpretation but also useful in extracting clinically relevant information from electronic patient records. The second study was significant in that the algorithm could detect multiple abnormalities in chest x-rays (useful in real world settings) and was validated multiple times using external data-sets. Coupled with these developments, we now have the FDA gearing up for the inevitable use of AI software in clinical practice by developing a draft framework anticipating modifications to AI medical software. Also, we now have medical professional bodies across the world welcoming the entry of AI in medicine albeit cautiously and by issuing guidelines. Like this one and this one. Compared to even a year ago, it seems AI has definitely had a resounding impact on healthcare. Even the venerable IEEE is keeping track of where AI is exceeding the performance of clinicians. However, I most certainly think we have yet seen the proper entry of AI in healthcare. Let me explain why and what needs to be done to enable this? While there is strong evidence emerging about the usefulness of machine learning, especially neural networks in interpreting multiple medical modalities, the generalization of such successes is relatively uncommon. While there has been progress with the ability to minimize generalization error (through avoidance of over-fitting) and understanding how generalization and optimization of neural networks work, it still remains the fact that prediction of class labels outside trained data sets is not for certain. In medicine, this means deep learning algorithms that have shown success in certain contexts are not guaranteed to deliver the same success even with similar data in a different context. There is also the causal probabilistic approach of current machine learning algorithms, which do not necessarily align with the causal deterministic model of diagnostic medicine. I have covered this issue previously here. Even if we accept that machine learning/deep learning models with current limitations are useful in healthcare, there is the fact there is limited readiness of hospitals/health services to deploy these models in clinical practice. The lack of readiness spans infrastructure, policies/guidelines and education. Also, governments and regulatory bodies in many countries don't have specific policies and regulatory frameworks to guide the application of AI in healthcare. So, what has to be done? As illustrated below, the following steps have to be adopted for us to see AI bloom in the healthcare context. The first step is development and use of appropriate AI Technology in Medicine. This means ensuring there is validity and relevance of the algorithms being used to address the healthcare issues. For example, if a convolutional neural network model has shown success in screening pulmonary tuberculosis through chest x-ray interpretation it doesn't necessarily mean it is equipped to identify other chest x-ray abnormalities say atelectasis or pneumothorax. So the model should be used for the exact purpose it was trained. Also, the model trained with a labelled x-ray data-set from a particular region has to be validated with a data-set from another region and context. Another issue that pertains to technology is the type of machine learning model being used. While deep learning seems to be in-vogue, it is not necessarily appropriate in all medical contexts. Because of the limitations it poses with explainability, other machine learning models like Support Vector Machines, which lend themselves to interpretability should be considered.
The second step in facilitating the entry and establishment of AI in healthcare is Infrastructure. What do I mean by infrastructure? At this stage, even in developed countries, hospitals do not necessarily have the digital platforms and data warehouse structures for machine learning models to successfully operate. Many hospitals are still grappling with the roll-out of electronic health records. This platform will be essential for machine learning algorithms to mine and query patient data. Also, to train many machine learning models structured data is necessary (some models can work on unstructured data as this application). This data structuring process includes data labelling and creating data warehouses. Not all hospitals, facing budget crunches, have this infrastructure/capability. Further, the clinical and administrative workforce and patient community are to be educated about AI if AI applications will be used in clinical practice and healthcare delivery. How many healthcare organizations have this infrastructure readiness? I doubt many. So infrastructural issues are most certainly necessarily to be addressed before one can think of use of AI in the healthcare context. The next step, Policy, is also critical. Policy covers both governmental and institutional strategies to guide the deployment of AI for healthcare delivery, and regulatory frameworks to facilitate the entry of and regulate AI medical software in the market. There is definitely progress here with many governments, national regulatory bodies, medical professional bodies and think tanks issuing guidance about this matter. Yet, there are gaps in that many of these guidance documents are theoretical or cursory in nature or not linked to existing infrastructure. Worse yet, is in countries where such policies and guidance don't exist at all. Also, an issue is limited funding mechanisms to support AI research and commercialization, which has significantly hampered innovation or indigenous development of AI medical applications. The final step that needs to be considered is Governance. This step not only covers the regulation frameworks at the national level (necessary to scrutinize and validate AI applications) but also monitoring and evaluation frameworks at the institutional level. It also covers the requirement to mitigate risk involved in the application of AI in clinical care and the need to create patient-centric AI models. The latter two steps are vital in clinical governance and continuous quality improvement. Many institutions have issued ethical guidelines for the application of AI in Healthcare, but I am yet to see clinical governance models for the use of AI in clinical care. It is critical that clinical governance models for the application of AI in healthcare delivery are developed. Addressing the steps, I list above: Technology, Infrastructure, Policy and Governance appropriately will most certainly facilitate the entry and establishment of AI in Healthcare. Also, with the accelerated developments in AI technology and increasing interest in AI by policy makers, clinical bodies and healthcare institutions, maybe we are not that far away from seeing this occur. |
AuthorHealth System Academic Archives
December 2023
Categories |

 RSS Feed
RSS Feed