Why healthcare systems should adopt A.I. in healthcare delivery? (Part 1-Economic Benefits)18/2/2018 (This article was first posted on LinkedIn)
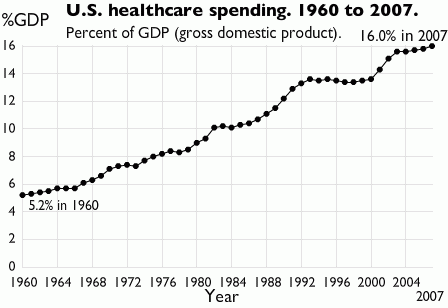
Keeping aside the buzz and hype about utilization of A.I.* in various disciplines and what mistakenly many assume it can accomplish, there are real merits in governments and decision-makers setting out strategies for adoption of A.I. in health service delivery. In this article, I will review the economic benefits of the application and in later articles, the other advantages. Of those health systems analyzed by the Commonwealth Fund in their performance rankings, people in the U.S. and Australia had the highest out-of-pocket costs when accessing healthcare. This issue has arisen not for the lack of investment in healthcare by governments in these countries. In 2016, the healthcare spending in the U.S. increased by 4.3 percent to attain a figure of US$3.3 trillion or about US$10,348 per person. Of the US$3.3 trillion, US$1.1 trillion was spent on hospital care, US$92 billion on allied health services and about US$162.5 billion on nursing care facilities and retirement communities. Together these expenditures constituted approximately 45% of the 2016 health spend. Of the total health expenditure, individuals/households contribution matched the government expenditure (28% of the total health expenditure). In Australia in 2015-16, the total healthcare spend was AU$170.4 billion (a AU$6 billion increase compared to 2014-15). Of this, the government expenditure on public hospital services was AU$46.9 billion and on primary healthcare AU$34.6 billion. Expenditure by individuals accounted for 52.7% of non-government expenditure or 17.3% of total health expenditure. While governments continue to increase spending this hasn't really made a serious dent on out-of-pocket costs. One of the key component of annual healthcare spending and pertinent to this article is the recurrent healthcare expenditure. Recurrent healthcare expenditure does not involve acquisition of fixed assets and expenditure on capital but largely expenditure on wages, salaries and supplements. In Australia, recurrent healthcare expenditure constitutes a whopping 94% of the total expenditure and in the US, about US$664.9 billion was spent on physician and clinical wages in 2016. Considering it is unlikely for wages to go down; it is hard to imagine recurrent healthcare expenditure decreasing and consequently total healthcare spend decreasing . A.I. technology, which has been around for decades but has only recently received wide-spread attention, is increasingly being applied in various aspects of healthcare (primarily in the U.S.). While in an earlier article, I have argued how A.I. can never totally replace human clinicians**, many number of American hospitals are using A.I. technology to leverage their consultants expertise where in some cases the A.I applications are outperforming them. I won't discuss the technologies and application here (as it will be covered in my book chapter^ and in subsequent articles) but I will discuss the costs of development of these technologies from a healthcare point of view. With traditional software development, the usual phases include discovery and analysis phase, prototype implementation and evaluation phase, minimum viable product and followed by product release. The costs associated with these phases, depending on the project sizes and complexity of the software, can constitute anywhere from US$10,000 to US$100,000^^. However, development of AI programs (here I will consider Machine Learning based programs not robotic applications, which adopt a different development model and consequently different cost models) have distinctive features to be considered in their development. These aspects include acquisition of large data sets to train the system and fine-tuning the algorithms that analyze the data. Where significant data sets cannot be obtained, data augmentation can be considered. Costs will be incurred in acquiring the data sets if not available in prior. However, in the context of healthcare government agencies and hospitals can provision this data for developers at no costs (if the A.I. program is being developed/customized for their exclusive use). So the most cost impacting factor is whether the data is structured or not. Data doesn't have to be structured, there are several machine learning algorithms that are trained to analyze unstructured data. However, developing programs to review unstructured data incurs more costs. Even when structured data is available, there are processes like data cleansing and data type conversion, which add to the costs. The next distinctive feature is fine-tuning/customizing the machine learning algorithm to suit organization's requirements. As the healthcare context requires the program to have a high degree of accuracy (less false negatives and high true positive identification epidemiological speaking), many round of refinements of the algorithm will be required. Even considering these distinctive features, which will add to the baseline costs ranging from US$50,000 to US$300,000^^; you are looking at a range of total costs of US$60,000 to US$500,000^^ (depending on the organisation requirements and complexity of the A.I. software). If we consider in the U.S. about US$664 billion (2016) and in Australia that AU$64 billion (2015-2016) was spent on hospital recurrent expenditure alone, a mere 0.016% allocation of the spend on developing A.I. technologies could fund development of at least 18 (hospital focused advanced machine learning based) applications per annum. The ROI is not just economic but also improvement in patient outcomes because of avoidance of medical errors, improved medical/laboratory/radiological diagnosis and predictability of chronic disease outcomes. Considering the rapid advances machine learning based program have made in medical prediction, diagnosis and prognosis^ , governments and healthcare organizations should seriously consider focus on supporting the development and deployment of A.I.technologies not only for the serious dent these applications can make on recurrent health expenditure but also how they can significantly improve patient access. Footnotes * I have a distaste for the term 'A.I.' which I have explained the reasons for in an earlier article but use this term as it is widely recognizable and accepted to portray computational intelligence based products. **https://www.linkedin.com/pulse/role-human-clinicians-automated-health-system-dr-sandeep-reddy/ ^ 'Use of Artificial Intelligence in Healthcare' (book working title: E-Health, ISBN 978-953-51-6136-3; Editor: Thomas.F.Heston, MD) ^^ This estimation does not take into consideration deployment, insurance and marketing costs.
0 Comments
Eric Topol, a Professor of Genomics and Cardiologist, in his 2015 NYTimes bestseller 'The Patient Will See You Now', foresees the demise of the current form of hospital based acute care delivery (with a shift to delivery of care at homes of patients) along with replacement of human delivered clinical services by smart systems/devices in the coming future. I would not go so far as Professor Topol in his assessment about the replacement of human clinicians but can easily foresee the automation of a large part of human led clinical care in the coming decades.
While I do not remotely purport to be an expert on automated medical systems (that will take some more time and neurons); having undertook months of research to complete a book chapter on the use of Artificial Intelligence in healthcare (book working title: E-Health, ISBN 978-953-51-6136-3; Editor: Thomas.F.Heston, MD), just completed a hands-on AI programming course delivered by Microsoft while undertaking a scoping review of the use of recurrent neural networks in medical diagnosis and preparing the use case of a non-knowledge based clinical decision support system, I can rationally state where the automation of healthcare delivery is heading to. Before I analyse the 'artificial intelligence take-over of medical care' scenario further, I would like to here express my slight distaste for the term 'Artificial Intelligence'. This term derives from the incorrect assumption intelligence has been primarily a biological construct so far and any intelligence that is now being derived outside the biological domain is artificial. In other words, intelligence is framed exclusively in reference to biologically derived intelligence. However, intelligence is a profound entity of it's own with defined characteristics such as learning and reasoning. Human intelligence is not the most intelligence can be and as trends go, computing programs with their increasingly advanced algorithms can potentially in the next decade or so exceed the learning and reasoning powers of humans in some aspects. Therefore, a source based terminology for intelligence would be more appropriate to frame intelligence. In other words, computational intelligence would be more appropriate than artificial intelligence. Healthcare has been a fertile domain for computational intelligence (CI) researchers to apply CI techniques including artificial neural networks, evolutionary computing, expert systems and natural language processing. The rise in interest and investment in CI research has coincided with the increasing release of CI driven clinical applications. Many of these applications have automated the three key cornerstones of medical care: diagnosis, prognosis and therapy. So it is not hard to see why commentators, including clinical commentators, are predicting the replacement of human clinicians by CI systems. While it is indeed rational, based on current trends in CI research, to imagine automation of many human clinician (for convenience sake, I am focusing on physicians rather than other professions such as nurses, allied health professionals) led tasks including interpretation of laboratory and imaging results (CI applications are already matching the radiologist's accuracy in interpretation of MRI, CT and Radiological images), predicting clinical outcomes (CI applications have successfully predicted acute conditions by reviewing both structured and unstructured patient data) and diagnosing various acute conditions (in fact the earliest CI applications, dating back to the 70's, already had this ability); it is hard to imagine CI systems completely replacing human clinicians in conveying diagnosis and discussing complex treatment regimens with patients, especially with high risk patients. There are some other areas where it is equally hard to foresee automation of clinical tasks such as some complex procedures and making final treatment decisions. So what is to come? I foresee a co-habitation model. A model that accepts the inevitable automation of a significant number of tasks that are currently performed by human clinicians (the at-risk areas are where there is less human interaction and where there is a structured process in implementing the task; structure means algorithms can be developed easier you see) but allows for human clinicians to make the final decision and be the lead communicator with patients. Bibliography E. Topol, The Patient Will See You Now: The Future of Medicine is in Your Hands. New York: Basic Books, 2015. J. N. Kok, E. J. W. Boers, W. A. Kosters, P. Van Der Putten, and M. Poel, “Artificial Intelligence: Definition, Trends, Techniques, and Cases,” 2013. D. L. Poole and A. K. Mackworth, Artificial Intelligence: Foundations of Computational Agents, 2nd Edition. Cambridge University Press, 2017. B. Milovic and M. Milovic, “Prediction and Decision Making in Health Care using Data Mining,” Int. J. Public Heal. Sci., vol. 1, no. 2, pp. 69–76, 2012. K. L. Priddy and P. E. Keller, Artificial Neural Networks: An Introduction. Bellingham: SPIE Press, 2005. S. C. Shapiro, Encyclopedia Of Artificial Intelligence, 2nd Editio. New York: Wiley-Interscience, 1992. R. Scott, “Artificial intelligence: its use in medical diagnosis.,” J. Nucl. Med., vol. 34, no. 3, pp. 510–4, 1993. |
AuthorHealth System Academic Archives
December 2023
Categories |
 RSS Feed
RSS Feed